Upcoming Gallbladder Surgery
Upcoming Gallbladder Surgery
Dr. Danthuluri’s greatest interest is in metabolic surgery for weight loss. That includes the sleeve gastrectomy, single anastomosis duodenal ileal bypass (SADI), and gastric bypass procedures. He also performs bariatric surgery and offers management of the Lap-Band and band removal as well as revisional surgery. *Revisional surgery included band removal, conversion of the sleeve to SADI – just to name a few. He is fellowship-trained in bariatric surgery and a fellow of the American Society of Metabolic and Bariatric Surgery (ASMBS).
What is the gallbladder and what does it do?
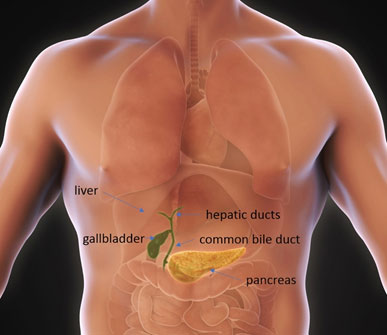
The gallbladder is a part of the hepatobiliary system. It is attached to the liver and it collects and stores bile that the liver constantly produces. Bile is important in the management of cholesterol elimination as well as elimination of bilirubin which is a byproduct of red blood cell recycling. The most important function as it pertains to the gastrointestinal system is in digestion. Bile helps to break down fats in the food you eat so that they can be absorbed along with certain vitamins like vitamins A,D,K and E.
When you eat a meal, especially a fatty or greasy meal, the cells in the intestine signal the gallbladder to squeeze and inject a large dose of bile into the intestine where it can mix and process that food. Liquid bile is easy for the gallbladder to store and to squeeze out into the bile ducts. The ducts transport the bile to the intestine. Thick bile, or sludge as we sometimes call it, is not easy for your gallbladder to squeeze out. Also bile flow can be obstructed by stones. Think of it this way – How much easier is it to drink water from a straw versus a thick milk shake? Isn’t it annoying to drink a smoothie when it’s not ground up properly and large particles block up the the straw? A gallbladder with sludge or stones struggles the same way.
Why are you having gallbladder dysfunction or symptoms?
Normally the gallbladder stores liquid bile only and if sludge or gallstones have formed then the gallbladder has to work really hard to deliver that bile. A gallbladder working against the resistance of bile or a blockage gets swelling and inflammation. So thick bile and stones are the reason for your symptoms. There are different types of stones. The most common stones are cholesterol stones which form when there is extra cholesterol floating around. That’s why you are more likely to get gallstones if you have an unhealthy weight or have recently lost a lot of weight. The most common patients to get gallstones are over 40 years old, and usually woman who have had children. Young normal weight people can get stones too and could have a different type of stone causing problems. There is a strong genetic component too.
Once you have gallbladder stones, or gallstones, that’s called cholelithiasis (ko-lay-Lith Eye Asis).
Depending on where the stones are you can have different problems going on, such as symptomatic cholelithias, choledocholithiasis (koley-doh-ko lith eye asis) or gallstone pancreatitis. You may also hear you have cholecystitis (koley-cyst-eye-tis) or biliary dyskinesia (dis-kin-easy-ah).
What are some of the common symptoms of gallbladder stones or other gallbladder problems?
- Abdominal pain, specifically under the right rib cage area and upper abdomen
- Nausea with or without vomiting
- Upset stomach
- Abdominal fullness or indigestion
- Sometimes fever
- Also possibly skin and eye color changes to yellow
- Pain that radiates to the right side or right shoulder
What is symptomatic cholelithiasis?
That’s a gallbladder with stones causing pain, nausea and or vomiting. Typical pattern of gallbladder pain, or biliary colic, is a steady or intermittent ache in the upper abdomen or right upper abdomen usually starting 30-60 minutes after a meal. The pain can last minutes or hours. Pain episodes can be severe enough that they drive you to the ER but it still doesn’t mean you need surgery right away. At this stage mild symptoms can be controlled or avoided with a low fat diet and occasional pain medicine. When there’s low levels of fat in the meal you eat the gallbladder is not stimulated to contract. This is one of the most common reasons to get the gallbladder removed preemptively to avoid repeat visits to the ER or to avoid some of the below more advanced complications of having gallstones.
What is cholecystitis?
That’s when the gallbladder outlet, the cystic duct, is blocked so bad and for so long that the gallbladder is now getting swollen and inflamed. Stagnant bile, like stagnant water, has a risk of getting infected. So if the bile flow is blocked for long enough you could get cholecystitis with an infection. If left untreated without antibiotics and or surgery the gallbladder can develop gangrene and sometimes can even rupture. This can be life-threatening.
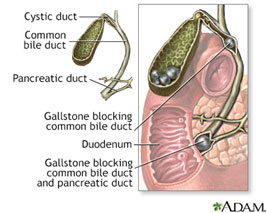
What is choledocholithiasis?
That’s when a stone has left the gallbladder and traveled into the common bile duct, which is a critical structure that drains both the gallbladder as well as the liver. When that happens it can not only block bile flow from the gallbladder but also from the liver itself. The liver can get damaged if blocked completely and for a long time. Bile back up in the liver can cause jaundice, yellowing of the eyes and skin. Again, when bile can’t flow freely for a prolonged period then it’s at risk for getting infected. If the common bile duct is infected, that’s called cholangitis (Kol-an-gytis)
This can be an emergency. Cholangitis is especially harmful and can cause rapid systemic illness. The stone needs to be removed and the gallbladder removed to eliminate the gallstones and avoid a recurrent episode.
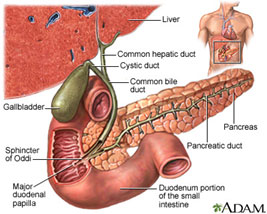
What is gallstone pancreatitis?
Very similar to above. It’s caused by a stone leaving the gallbladder and not just blocking the common bile duct but also blocking the pancreatic duct. The pancreatic duct drains the pancreas. Critical digestive enzymes need to leave the pancreas to mix with the food and break it down into other components (carbs and proteins, for example) for absorption. When the pancreatic duct is blocked the pancreas can get swollen and inflamed.
This can also be an emergency. The stone needs to be removed and the gallbladder removed to eliminate the gallstones and avoid a recurrent episode.
What is biliary dyskinesia?
This is when the gallbladder does not have stones, sludge, enlargement or inflammation necessarily, but is just not working optimally. If the gallbladder can’t generate enough “squeeze” to empty the bile then it can cause symptoms too. You’ll want your doctor to be sure there’s no other cause of your symptoms before taking on the risk of surgery to remove the gallbladder.
How do we identify gallbladder problems?
This is most commonly done by simple ultrasound, just like we use to study a growing baby in expecting mothers. The ultrasound study takes about 30 minutes. It will show the gallbladder itself and show if it is enlarged or thickened. It will find the stones and tell us how many and their sizes. It will show the ducts and their sizes too. We can also gather some information about the liver and other abdominal organs. Other studies that show gallbladder problems are CT scan, MRI or a HIDA scan. The CT scan can show an enlarged gallbladder and inflammation signs but may miss stones. An MRI is excellent for finding choledocholithiasis and gallstone pancreatitis. Finally a HIDA is the confirmatory study for cholecystitis, although not mandatory for diagnosis, and is the key study for diagnosing biliary dyskinesia.
How do we treat gallbladder problems?
Surgery to remove the gallbladder is the best treatment for the various gallstone diseases above. I’ll cover the technical aspects of surgery and pre and post operative expectations below. In some instances you may need a non-surgical procedure, called an ERCP, so I’ll discuss that briefly first.
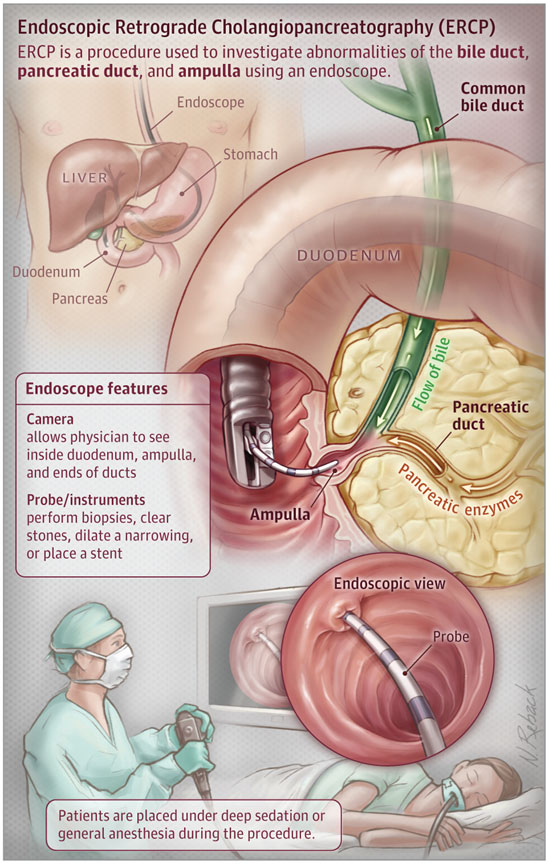
What’s an ERCP?
Technically that’s short for Endoscopic Retrograde Cholangiopancreatography. The Gastroenterologist is trained to do this procedure. It is most commonly performed for choledocholithiasis or gallstone pancreatitis to remove the common bile duct stones. Typically this is done first to remove the stone and alleviate the more emergent process (jaundice, pancreatitis or cholangitis) causing your symptoms and to save the pancreas and liver from permanent damage.
Sometimes if a stone is found in the common bile duct during surgery and it can’t be removed at the time of surgery, then you may need an ERCP after surgery.
How is the gallbladder removed?
Gallbladder removal is called cholecystectomy (Koley-cyst-ectomy). I can offer minimally invasive gallbladder removal techniques to my patients. Minimally invasive surgery includes robotic or laparoscopic cholecystectomy. These days open surgery is reserved for complications during minimally invasive surgery or for patients that can’t undergo robotic or laparoscopic surgery, usually because they have advanced heart disease.
Before Surgery:
*Note actual preopearive instructions can vary from patient to patient. I will discuss specifics with you if indicated.
The night before surgery you can’t eat any solid food after midnight. That’s a general anesthesia requirement. A limited amount of water for critical medications (such as heart medications) the morning of surgery is usually fine. We will review critical medications as needed but if you have concerns about missing medications the day of surgery, then be sure to ask before.
One thing I want all my patients to know is that surgery does hurt! Surgery requires cutting the skin, cauterizing blood vessels, and spreading tissues. There’s no avoiding some pain but I try to make the experience overall less painful than the problem for which we are doing surgery. Even then, sometimes surgery hurts worse than the problem itself, but only temporarily.
As much as possible I try to have my patients comply with an Enhanced Surgical Recovery (ESR) or Enhanced Recovery After Surgery (ERAS) protocol. These protocols were designed to look at safety and satisfaction outcomes after surgery and have proven to make the recovery period as safe and short as possible. The basic benefits are faster recovery, fewer complications and minimized opioid use. Opioid narcotic pain medications can slow recovery. Many people get drowsy, nauseated, and constipated while using narcotic pain medications. Research has proven that narcotics are often times not needed for post operative pain control.
To optimize pain control without these unwanted side effects I prescribe three non-narcotic pain medications to use after surgery. I will provide these in a written prescription before surgery or we will call them in to your pharmacy. These medications cover the general pain receptors, combat inflammation and target the nerves themselves that transmit pain signals. In my experience over 90% of patients have satisfactory pain control after their surgery with these medications. If needed, more medications including narcotic pain medications, can be prescribed. I always want you to be comfortable but we do not target zero pain after surgery. That’s not safe and can cause complications.
The morning of surgery you will arrive at the hospital about 2 hours before scheduled surgery. You will get prepared for surgery and meet your surgery team. That includes your preoperative nurse, the anesthesiologist and his or her team, as well as members from the surgery team. We will make sure you are comfortable and as stress-free as possible. You will have an IV established to give anesthesia medications and IV fluids. You will sign some final paperwork. Importantly the consent form for surgery needs to be signed if it wasn’t signed in the office. You won’t go anywhere without seeing me before surgery. We will have a chance to address final questions and for me to meet your accompanying family member, spouse or close friend.
During Surgery:
I always say that a surgery takes as long as is needed to be done safely and effectively. However typically the surgery will take one to two hours total. If there is a lot of inflammation or scar built up for any reason this could add time to the surgery to be done safely. Rarely surgery takes longer than three hours. Whether or not we have to do a procedure during surgery called a cholangiogram (Cole-Angie-O-gram) also will add time to the surgery. A cholangiogram is when, prior to removing the gallbladder, we inject a special contrast material directly into the bile ducts to study them and make sure there is no gallstone stuck in the common bile duct. This requires a special machine which uses basic x-ray technology to show us the images we need to see. So there is a minor X-ray radiation exposure during the surgery for you to be aware of, and please note that we really limit the duration and frequency of radiation exposure as able during a cholangiogram. Overall for reference this is similar to getting a series of x-rays for a broken bone, if you have had that done before.
The Surgery is performed with four to five small incisions across the abdomen. Final location of incisions varies from patient to patient and depending on if we are doing a laparoscopic or robotic surgery. See the images below for typical incision placement. Usually for robotic surgery the incisions are diagonal across the abdomen and I try to put the largest incision, the gallbladder extraction site, partially buried in the belly button. Sometimes if your body habituate allows for it, the incisions can all be low along the waist line so they are completely hidden. I try my best to use the smallest possible incision I can and hide them as able. I will also try to use old scars if you have had surgery before. However I will not sacrifice safety for cosmetic satisfaction. Three of the incisions will be about 1-1.5 cm (~0.5 in) and the gallbladder extraction site, depending on how big the gallbladder and stones are, may need to be 3-4cm long (~1.5 in). Also note that the inside portion of the extraction site incision could be even longer than it appears on the outside. This site will usually require one or two deeper stitches down in the abdominal muscle layer to keep it closed and to prevent an incisional hernia in the future. This is also the site of most of the post operative pain. Finally a tiny, less than 1cm, incision may be used to complete that cholangiogram when needed.

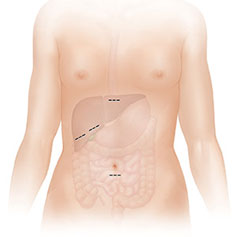
The above pictures are a picture of laparoscopic surgery. Note the incisions are in a square pattern in the right upper corner of the abdomen.
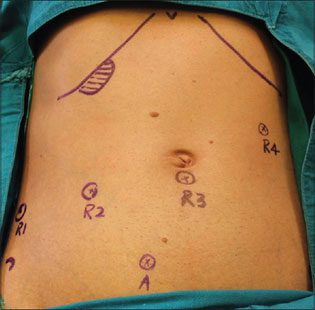
This image shows the typical location of incisions for a robotic cholecystectomy. Diagonal across the abdomen. R1-R4 are the robotic instrument sites. The “A” represents a possible assistant port site but we usually don’t need that one. As I said above, if your body habituate allows for it, those robotic instrument incision sites will all be moved lower, close to the waistline.
